 Researchers in Jerusalem have found they can test for antibiotic resistance to better treat sepsis and even target cancer treatments better
Researchers in Jerusalem have found they can test for antibiotic resistance to better treat sepsis and even target cancer treatments better
Is it just us or do we seem to get sicker and sicker every winter? This last few months we have been at home sick more than we have been without. Indeed superbugs like the bird and swine flu virus H1N1 are reported to be going around, suggesting why everyone is getting a vaccine to try and beat it. But that’s a virus. When it comes to bacterial infections antibiotics are the only relief.
Every year in the United States, more than 35,000 people die and 2.8 million get sick from antibiotic-resistant infections. The medicine we have isn’t good enough.
Israeli tech to tackle bacteria resistant to antibiotics
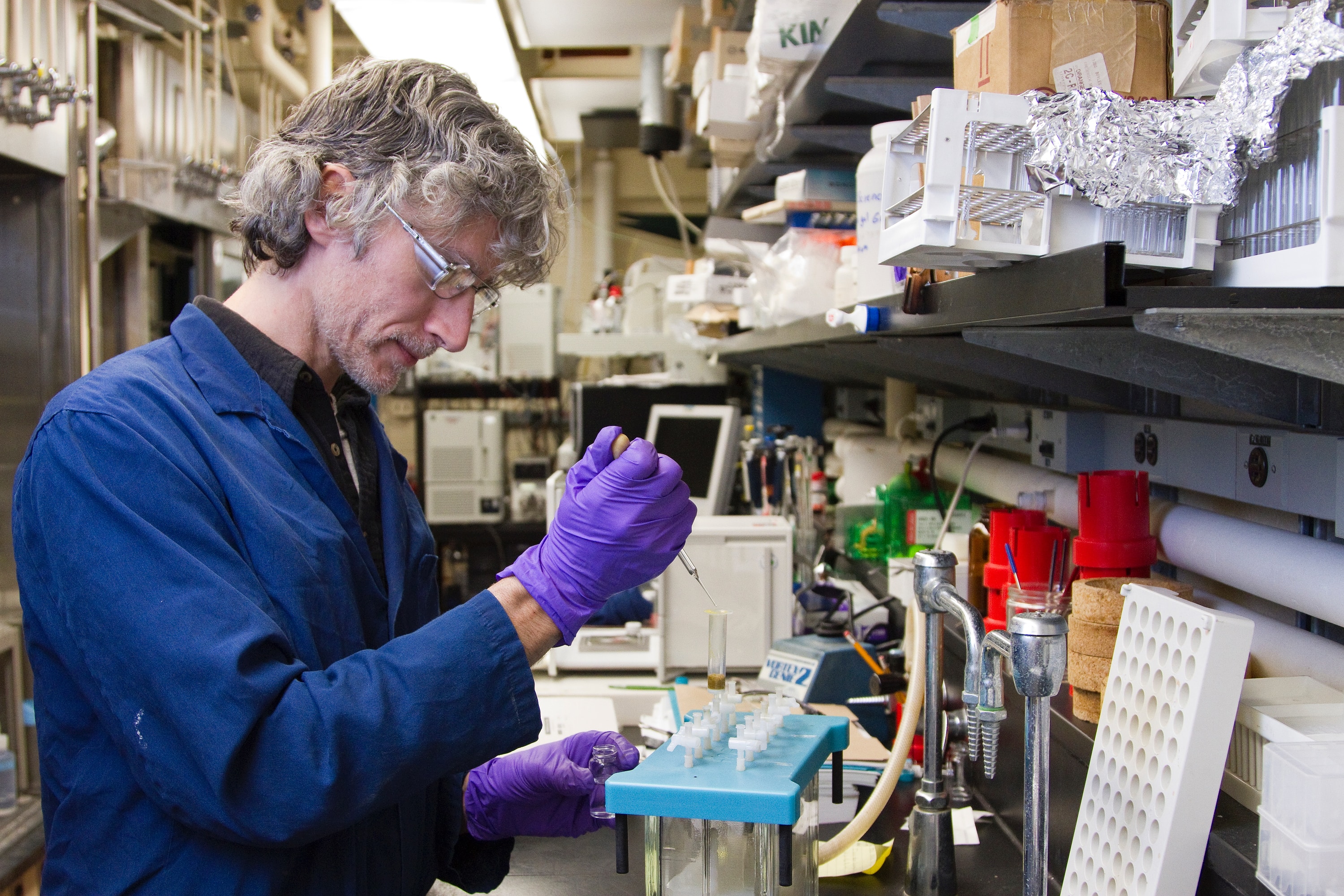
But new research may prevent some unwanted deaths due to infections like pneumonia. It is published in the prestigious journal Scient. The team led by Hebrew University of Jerusalem (HU)’s Professor Nathalie Balaban and Shaarei Zedek Medical Center’s Dr. Maskit Bar-Meir describe their approach.
Like all living organisms, germs like bacteria develop defenses against hostile elements in their environment. One common tactic is “tolerance”, that is, lying dormant during antibiotic treatment. In this way, bacteria evade antibiotic treatment because antibiotics can only spot and kill growing targets. However, this intermediary stage called “antibiotic tolerance” lasts only a few days and cannot be detected in standard medical labs. Therefore, doctors miss the tolerance window and with it the opportunity to treat a serious infection before it becomes altogether resistant. This short window does not affect most healthy adults but for those patients fighting off a blood infection with a weakened immune system, this window is critical and could mean the difference between life and death.
Math tests if antibiotics will be effective
In a previous study, Balaban and student Irit Levin-Reisman studied lab-controlled bacteria. They developed a mathematical model that successfully described, measured and predicted when bacteria would develop tolerance to a particular antibiotic.
Further, they observed that when bacteria developed tolerance to one antibiotic, they were more likely to develop tolerance to other antibiotics in the cocktail. “We observed that bacteria acquired tolerance within a few days. These tolerance mutations then acted as a stepping stone to acquire resistance and, ultimately, treatment failure,” described Balaban.
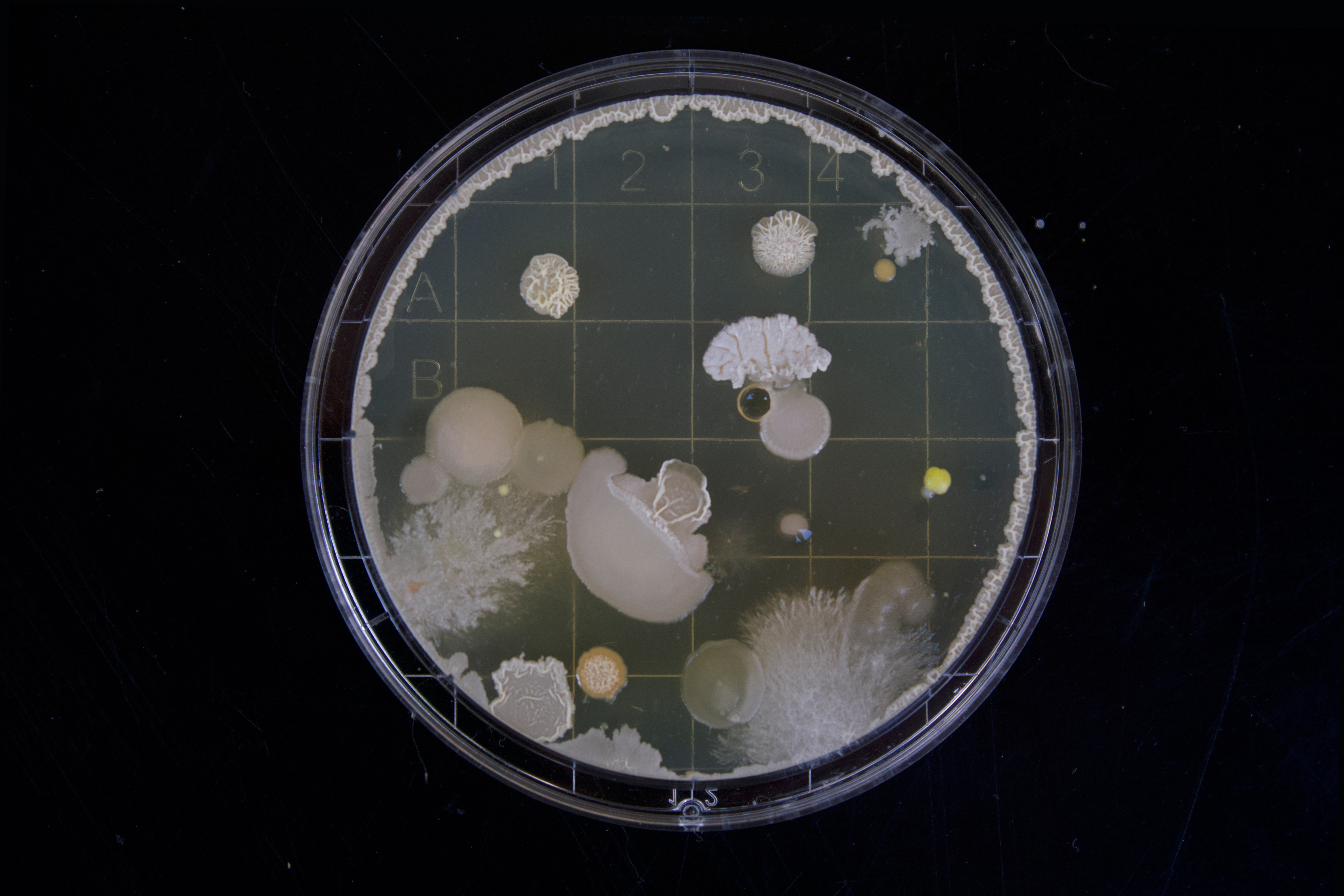
Now, as published in the latest edition of Science, HU’s Balaban lab and Dr. Jiafeng Liu teamed up with Bar-Meir and repeated their study and tolerance test technique. Only this time, they analyzed daily bacterial samples from hospitalized patients with life-threatening, persistent MRSA (methicillin-resistant Staphylococcus aureus) infections. The pattern that they found was strikingly similar to their lab findings: First, the patients’ bacteria developed tolerance, then resistance, and ultimately antibiotic treatment failed.
Applications for testing in cancer treatment
Looking ahead, Balaban believes that the same evolutionary processes involved in the development of antibiotic tolerance and resistance are likely at play in cancer and might be used to inform treatment. For example, tumor cells might first become tolerant of chemotherapy, develop resistance to it, and then develop resistance to other cancer drugs, as well.
In the short term, Balaban and Bar-Meir would like to give new hope for patients with life-threatening infections by encouraging medical centers to adopt the laboratory test they developed which gauges antibiotic tolerance.
This readout would enable doctors to quickly and easily detect whether a patient’s bacteria are tolerant of a planned antibiotic treatment before it’s administered. Further, based on the patient’s bacteria profile, doctors could handpick antibiotics with a greater chance of success that, as is currently done, blindly choose antibiotics for which the patient may have already developed a tolerance.
“Using the right combination of available antibiotic drugs at the outset could dramatically increase a patients’ survival rate before their infection becomes tolerant to all the antibiotics in our arsenal,” Balaban concluded.



